Upper Intestine Pain Gastrointestinal Distress
- 1.
What Exactly is "Upper Intestine Pain" – A Misnomer We Keep Whispering Over Tea?
- 2.
Why Do My Upper Intestines Hurt? — Peeling Back the Layers Like a Suspicious Onion
- 3.
When the Pain Sits High Under the Ribs: Anatomy’s Little Deception
- 4.
The Stabbing Pain in the Upper Centre of the Abdomen: Not Just a Plot Twist in a Medical Drama
- 5.
Symptoms of Epigastric Pain — More Than Just a Grumble After Sunday Roast
- 6.
Diet, Stress & That One Pint Too Many — Lifestyle Triggers We Pretend Don’t Exist
- 7.
Diagnosis — Not Guesswork, but Proper Detective Work
- 8.
Treatment — From Antacids to Actual Healing
- 9.
When It’s Not the Gut — Cardiac, Pulmonary, Even Musculoskeletal Mimics
- 10.
Living With (and Preventing) Upper Intestine Pain — Because Nobody Wants a Repeat Performance
Table of Contents
upper intestine pain
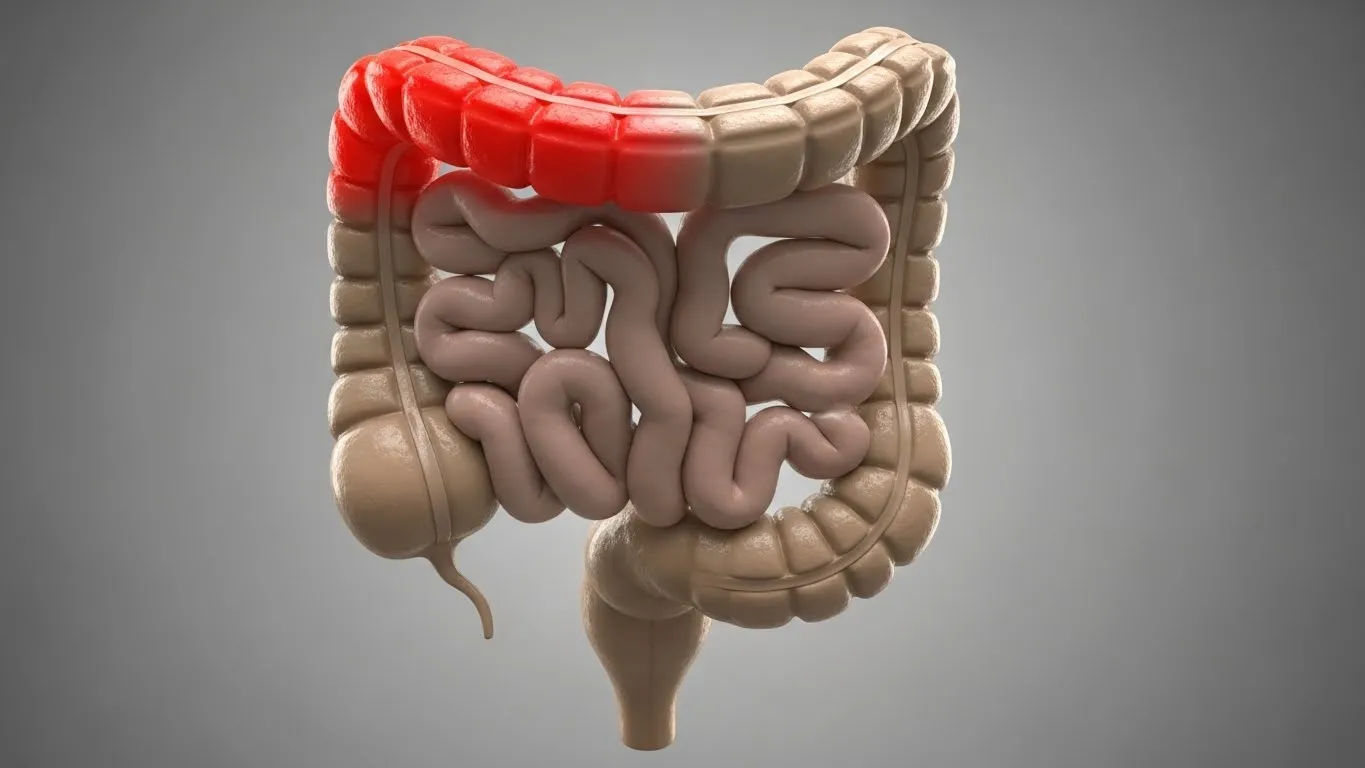
What Exactly is "Upper Intestine Pain" – A Misnomer We Keep Whispering Over Tea?
Ever woken up with a gnawing, almost theatrical ache nestled just beneath your ribs — like your belly’s auditioning for a Victorian melodrama? “Blimey, is it the upper intestine again?” you mutter, clutching the hot water bottle like it’s the last bus home. Truth be told, there ain’t no actual “upper intestine” per se — not in proper anatomy textbooks, at least. The small intestine *does* start just past the stomach (duodenum, jejunum, ileum — rollin’ off the tongue like a pub quiz champ), but when folks moan about upper intestine pain, they’re usually pointing at that epigastric zone: the soft dip beneath the sternum, where ribs part ways like polite commuters at a Tube station. Medics raise an eyebrow & say “epigastric discomfort,” but we? We feel it as a sharp twinge, a dull burn, or a full-blown *stabbing pain in the upper centre of the abdomen* that makes you whisper sweet nothings to your antacid sachets. It’s the body’s cryptic Morse code — and we’re still fumbling with the decoder ring.
Why Do My Upper Intestines Hurt? — Peeling Back the Layers Like a Suspicious Onion
If your upper intestine pain feels like someone’s tightened a belt two notches too far, or like a tiny badger’s doing parkour behind your ribcage — congrats, you’ve entered the murky lobby of gastrointestinal distress. Causes? Oh, they’re as varied as the pints on tap at a proper London boozer. Could be something as mundane as acid reflux — especially if you polished off a vindaloo and a double stout last night — or as serious as a peptic ulcer chiselling away at your duodenum. Gallstones? Yep, they love to throw surprise parties under your right rib. Pancreatitis? Less festive, more like a fire alarm blaring at 3 a.m. Even functional dyspepsia — a posh way of saying “your gut’s in a mood & no one knows why” — can masquerade as upper intestine pain. One chap we spoke to swore it was stress; turns out, his cortisol levels were higher than the Shard on a foggy morning. So: *why do my upper intestines hurt?* Likely because your upper GI tract’s staging a one-man protest — and it’s picketing *right* under your xiphoid process.
When the Pain Sits High Under the Ribs: Anatomy’s Little Deception
Ah, the classic complaint: “Why does my stomach hurt high up under my ribs?” Bless. It *feels* like your stomach’s gone rogue and migrated north, but let’s get anatomical, shall we? That tender pocket beneath the costal margin? It’s not the stomach *itself* misbehaving — well, not always. The duodenum (first bit of small intestine), pancreatic head, gallbladder neck, even the lower oesophagus — all squished in there like commuters in a rush-hour Overground carriage. A hiatal hernia can shove part of the stomach *up*, yes — but often, upper intestine pain radiating high under the ribs is duodenal in origin. Think of it like faulty wiring: one short circuit in the duodenum, and the alarm bell rings in the epigastrium. One bloke described it as “a rugby tackle from the inside.” Spot on, mate. The diaphragm’s dome sits right there too — so irritation? Referred pain? Oh, it’ll play tricks. Your belly’s got layers, like a proper trifle: custard on top, but jam *and* sherry somewhere deeper down.
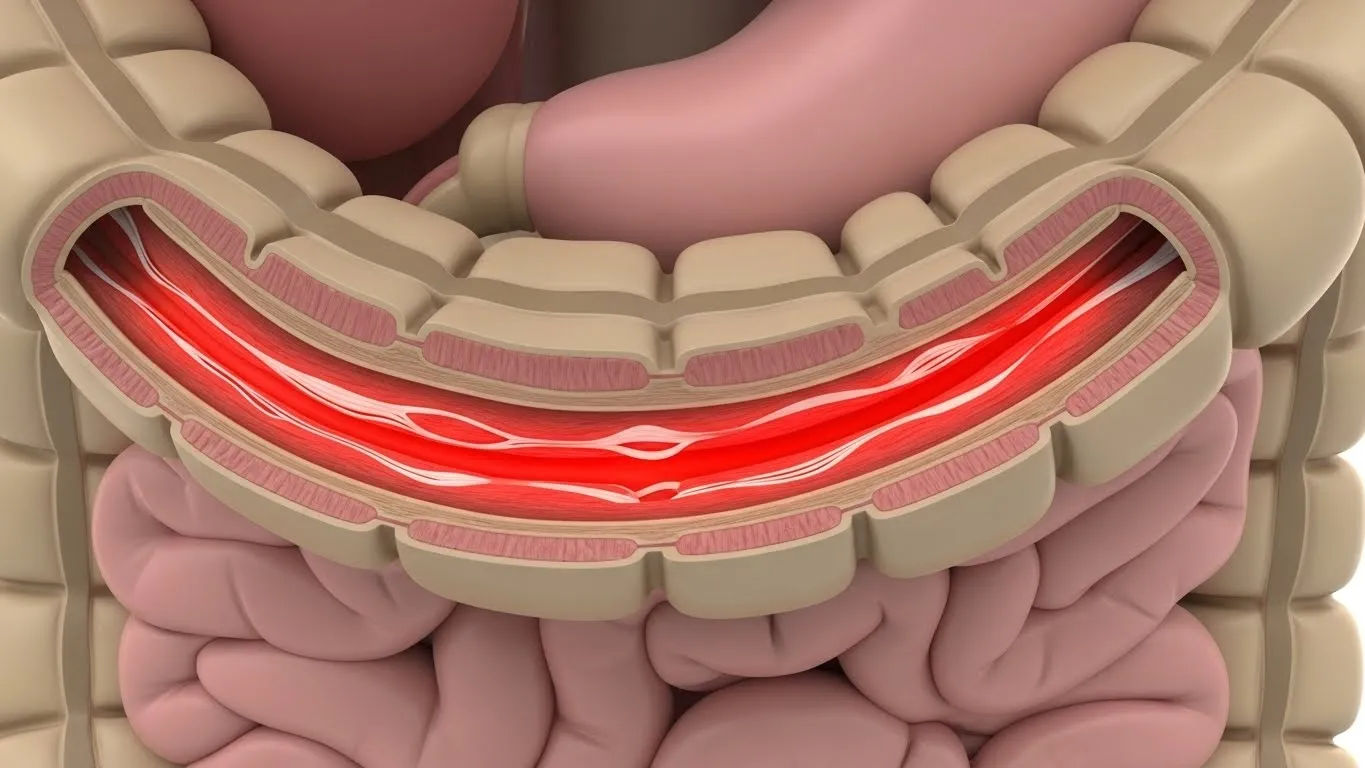
The Stabbing Pain in the Upper Centre of the Abdomen: Not Just a Plot Twist in a Medical Drama
Let’s talk about *that* sensation — sudden, sharp, makes you freeze mid-sip of Earl Grey like you’ve just remembered you left the iron on. The stabbing pain in the upper centre of the abdomen is no joke. It’s often visceral pain — meaning it’s coming from organs, not muscles — and the nerves there don’t localise well, so your brain just goes, *“Centre stage. Emergency lighting. Now.”* Classic culprits? Perforated ulcer (think: acid burning through tissue like a rogue sparkler), biliary colic (gallstone wedged in the cystic duct — ouch), or acute pancreatitis (enzymes digesting *you* instead of your lunch). One ER doc told us: “If it’s so sharp they double over and whisper *‘not again’* — we scan, stat.” Don’t shrug it off as “just gas.” If your upper intestine pain feels like a letter opener’s lodged behind your sternum? Phone NHS 111. Or better — A&E. No shame in it.
Symptoms of Epigastric Pain — More Than Just a Grumble After Sunday Roast
Right, so what else tags along when upper intestine pain comes to tea? It’s rarely solo. Think of it as the lead singer in a dodgy pub band — always brings backup: bloating that makes your jumper feel two sizes too small, nausea that lingers like an unwelcome relative, early satiety (you push away the shepherd’s pie after three bites — *unheard of!*), maybe even heartburn that tastes like battery acid and regret. Some folks get referred pain — say, between the shoulder blades (thanks, gallbladder), or radiating to the back (pancreas waving a red flag). Here’s a quick snapshot of common red-flag combos:
| Symptom Cluster | Possible Underlying Cause | Urgency |
|---|---|---|
| Burning + worse after meals + night waking | Duodenal ulcer | High — risk of perforation/bleed |
| Sharp + right upper quadrant + fatty food trigger | Biliary colic / cholecystitis | Medium-High |
| Constant dull ache + back radiation + vomiting | Pancreatitis | High — needs admission |
| Pressure-like + breathlessness + jaw pain | Cardiac ischaemia (yes, *heart*!) | EMERGENCY |
Don’t ignore weight loss, vomiting blood (‘coffee-ground’ or fresh red), or black tarry stools — those are the body’s neon signs flashing: *“CLOSED FOR REPAIRS. CALL PROFESSIONALS.”* Your upper intestine pain shouldn’t come with a side of existential dread — unless it’s *actually* urgent.
Diet, Stress & That One Pint Too Many — Lifestyle Triggers We Pretend Don’t Exist
Let’s be real: sometimes the culprit’s not a sinister pathology — it’s *us*. That third IPA? The midnight cheese toastie? The fact you’ve been scrolling job boards till 2 a.m. for three weeks straight? Stress ramps up cortisol, which cranks up gastric acid like it’s got a grudge. Fatty, spicy, acidic foods? They relax the lower oesophageal sphincter faster than a politician dodges a tough question. Alcohol? Oh, it’s a triple threat: irritates mucosa, boosts acid, *and* slows gastric emptying. One nutritionist we chatted with said, “I’ve seen more upper intestine pain cases linked to ‘weekend warrior eating’ than actual ulcers.” She’s not wrong. Even *overeating* — especially post-Christmas — stretches the stomach, triggers reflux, and voilà: epigastric fireworks. Try keeping a symptom diary. Note down meals, stress levels, sleep — patterns emerge faster than pigeons at Trafalgar Square at lunchtime.
Diagnosis — Not Guesswork, but Proper Detective Work
No, love, your GP won’t just hand you Gaviscon and send you off with a “chin up.” Proper workup for persistent upper intestine pain starts with history — *when* does it happen? *what* makes it better/worse? — then moves to tests. Bloods (amylase, lipase, LFTs, H. pylori serology), ultrasound (gallbladder’s first port of call), and if red flags? Straight to endoscopy (OGD — oesophagogastroduodenoscopy). Fancy word, but it’s just a tiny camera down the hatch to see what’s what. Stats? Roughly 60% of chronic epigastric cases get a functional diagnosis (dyspepsia); 25% structural (ulcer, gastritis); 15% need deeper digging. One study even found *H. pylori* in ~40% of uninvestigated dyspepsia in the UK — treat it, and symptoms vanish like fog on the Thames at noon. So don’t skip the scan. Your gut’s not a black box — it’s a vault. And we’ve got the key.
Treatment — From Antacids to Actual Healing
Slapping a PPI (proton pump inhibitor) on every twinge? Tempting — but not always wise. If it’s functional dyspepsia, low-dose antidepressants (like amitriptyline) can dial down visceral hypersensitivity — yes, really. For proven ulcers? PPIs *plus* *H. pylori* eradication (triple therapy: two antibiotics + PPI). Gallstones causing recurrent upper intestine pain? Cholecystectomy’s often the cleanest fix — laparoscopic, day case, back to tea & biscuits by teatime. Pancreatitis? Nil by mouth, IV fluids, then address the cause (alcohol? gallstones?). And lifestyle? Non-negotiable. Smaller meals. No late-night fry-ups. Elevate the head of your bed — gravity’s your mate. One NHS nurse whispered: “I tell my patients: treat your gut like a vintage Bentley. No cheap fuel. No redlining.” Wise words.
When It’s Not the Gut — Cardiac, Pulmonary, Even Musculoskeletal Mimics
Here’s the kicker: that upper intestine pain might not be gut-related *at all*. Angina can masquerade as indigestion — especially in women or diabetics (“silent ischaemia” they call it, like a spy in a trench coat). Pleurisy? Sharp, breath-dependent, worse when you cough. Costochondritis? Reproducible tenderness when you press the rib cartilage — feels like a bruise you didn’t earn. Even shingles (pre-eruption) can cause burning epigastric pain — unilateral, band-like, *before* the rash shows up. One bloke came in convinced it was “another ulcer flare” — turned out it was a small PE. Moral? If pain’s new, severe, or comes with sweating, dizziness, or shortness of breath — *think beyond the belly*. The body’s a master of disguise. Don’t fall for it.
Living With (and Preventing) Upper Intestine Pain — Because Nobody Wants a Repeat Performance
So how do we keep the peace with our upper GI tract? Prevention’s cheaper than endoscopy — and less awkward. First: eat like you mean it. Chew. Slow down. No scoffing at your desk like a startled squirrel. Second: know your triggers. Coffee? Chocolate? Mint? (Yes, *mint* relaxes the sphincter — ironic, innit?) Third: manage stress — not with another pint, but with walks, breathwork, or just sitting quietly with a cuppa and no screens. Fourth: don’t lie down within 3 hours of eating. Gravity’s free therapy. And fifth? Don’t self-diagnose on WebMD at 2 a.m. — you’ll convince yourself you’ve got porphyria *and* lupus *and* a tapeworm. If upper intestine pain keeps knocking, get it checked. Early intervention = fewer complications. For more on gut health, swing by Riding London, dive into our Learn section, or read our deep-dive on referred patterns in Abdominal Pain With Back Pain: Referred Pain Link.
Frequently Asked Questions
Why do my upper intestines hurt?
Though “upper intestine” isn’t a technical term, upper intestine pain usually refers to discomfort in the epigastric region — often caused by issues in the duodenum (first part of the small intestine), stomach, gallbladder, or pancreas. Common triggers include acid reflux, peptic ulcers, gallstones, functional dyspepsia, or even stress-induced visceral hypersensitivity. Persistent or severe upper intestine pain warrants medical evaluation to rule out serious conditions.
Why does my stomach hurt high up under my ribs?
Pain high under the ribs — especially centrally or to the right — is frequently linked to organs tucked beneath the costal margin: the duodenum, gallbladder, liver edge, or pancreatic head. Conditions like biliary colic (gallstones), duodenitis, or a hiatal hernia can refer pain to this zone. Referred pain from the diaphragm or even cardiac issues may also present here. Don’t assume it’s “just indigestion”; recurrent upper intestine pain in this location needs proper imaging and assessment.
What are the symptoms of epigastric pain?
Epigastric pain — our colloquial upper intestine pain — often comes with bloating, early fullness, nausea, heartburn, or belching. Alarm symptoms include unintentional weight loss, vomiting (especially blood or coffee-ground material), black/tarry stools, or pain radiating to the back or jaw. If epigastric discomfort wakes you at night or worsens with meals, it could signal ulcer disease or gallbladder pathology. Track your symptoms — patterns help clinicians crack the case.
What is the stabbing pain in the upper center of the abdomen?
A sharp, stabbing pain in the upper centre of the abdomen (epigastrium) is a red flag for visceral emergencies: perforated peptic ulcer, acute cholecystitis, biliary colic, or pancreatitis. Less commonly, it may signal aortic dissection or myocardial ischaemia — especially if accompanied by sweating, pallor, or shortness of breath. This type of upper intestine pain demands urgent evaluation; don’t wait to see if it “settles down.” When in doubt, head to A&E — better safe than sorry.
References
- https://www.nhs.uk/conditions/stomach-ache/
- https://cks.nice.org.uk/topics/dyspepsia-and-gastro-oesophageal-reflux-disease/
- https://www.bsg.org.uk/guidelines/
- https://patient.info/digestive-health/upper-abdominal-pain





