Lower Gut Pain Digestive System Discomfort
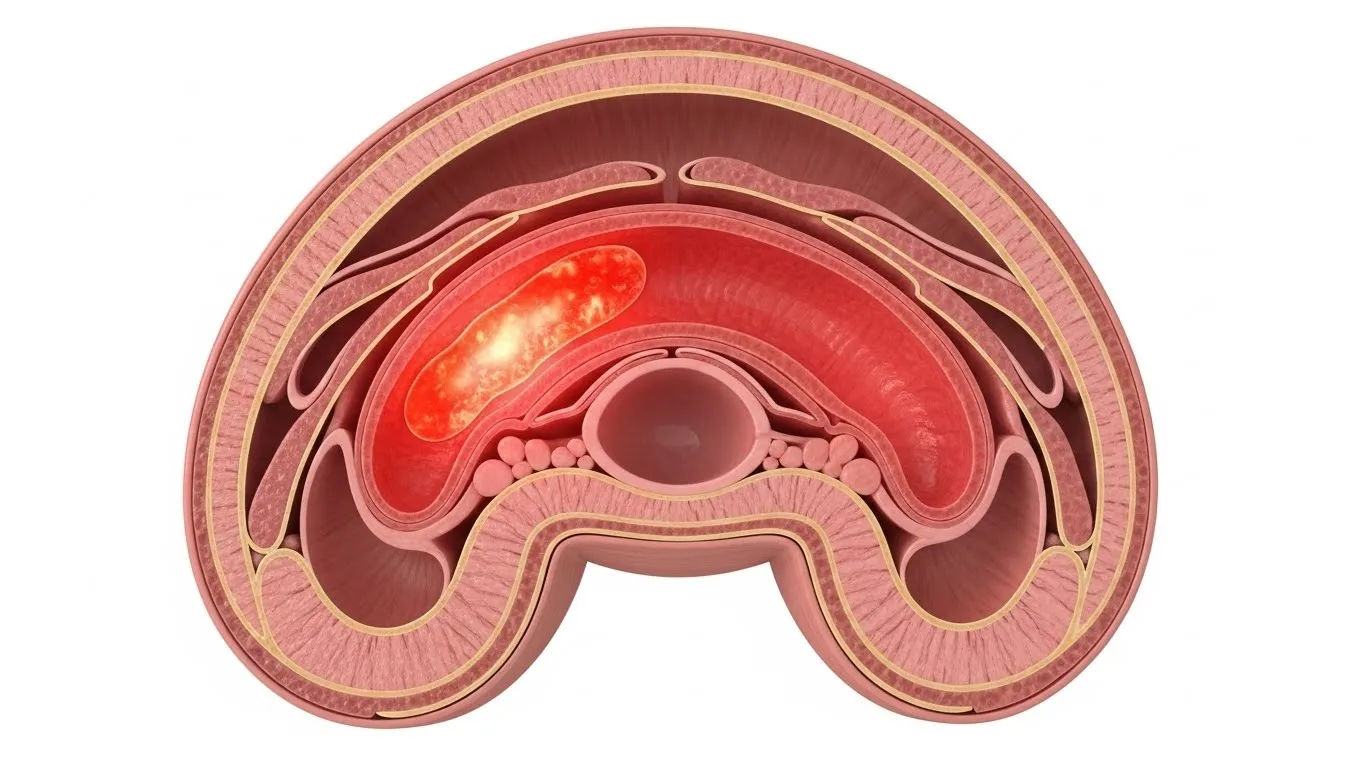
Table of Contents
lower gut pain
When Your Belly Starts Arguing with You—and Losing
Ever sat down for a cuppa, took a sip, and *bam*—yer lower belly staged a full-blown protest? Not a grumble. Not a whisper. A proper, *“Oi! We’re not happy down here!”* sort of ache—deep, dull, maybe crampy, maybe stabbing, maybe just… *persistent*? Yeah. lower gut pain doesn’t knock. It kicks the door in, makes itself tea, and refuses to leave till you listen. We’ve all had it—the “tummy bug” that’s suspiciously timed with that dodgy kebab, or the monthly visitor who brings a suitcase of discomfort. But sometimes? It lingers. Shifts. Radiates. And that’s when the little voice in yer head pipes up: *“Right. What’s actually going on down there?”* Spoiler: it’s rarely one thing. But it’s *always* worth paying attention to.
Anatomy Refresher: Where Exactly Is the “Lower Gut”, Anyway?
Let’s get anatomical—but not *too* anatomical. Think of yer abdomen as a flat with three floors: upper (stomach, liver, pancreas), middle (small bowel), and lower (large bowel, bladder, reproductive bits). The lower gut mainly means the *colon*—specifically the descending colon, sigmoid colon, and rectum—plus the terminal ileum (the small intestine’s handover zone). When folks say “lower gut pain”, they usually mean *below the navel*, often left-sided (sigmoid colon’s postcode: LLQ), but sometimes central or right (caecum’s turf). Important: the gut’s got *visceral* nerves (vague, hard-to-pinpoint ache) *and* *parietal* ones (sharp, localised—if inflammation reaches the peritoneum). That’s why some pain feels like a deep rumble… and others like someone’s poking ye with a knitting needle.
Common Culprits: From “Meh” to “Call the Doc”
Right—let’s play detective. Most lower gut pain falls into buckets. Here’s the usual suspects:
- Irritable Bowel Syndrome (IBS): Crampy, relieved by poo, linked to stress/food. No structural damage—just a hypersensitive gut throwing a strop.
- Diverticular disease: Small pouches (diverticula) in the colon wall—common >50yrs. Can inflame (diverticulitis), causing *constant*, left-sided pain + fever.
- Inflammatory Bowel Disease (IBD): Crohn’s or UC—chronic inflammation. Pain + bloody diarrhoea + weight loss. Not to be ignored.
- Constipation: Simple, yes—but a rock-hard stool in the rectum? Feels like pressure, bloating, even *false* urgency.
- Gynaecological causes: Endometriosis (cyclical, deep), ovarian cysts (sudden twist = surgical emergency).
Less common—but vital: bowel obstruction, ischaemia (reduced blood flow—*medical emergency*), or even referred pain from the spine. Context *matters*. Duration? Triggers? Pattern? That’s yer first clue.
What Does Pain in the Colon *Actually* Feel Like?
Ah, the million-quid question. Colon pain’s a shapeshifter:
- IBS-type: Crampy, colicky—comes in waves, eases after bowel movement. Often bloating + gas. May alternate diarrhoea/constipation.
- Diverticulitis: Steady, *deep*, left-lower-quadrant ache—worsens over days. Tender to touch. Fever? Nausea? Red flags.
- Colitis (infectious or IBD): Cramping + urgency + frequent loose stools—*often bloody*. Feels like “I need to go *now*… but nothing comes.”
- Obstruction: Intermittent cramps → *constant* pain, distension, vomiting, *no flatus*. “Sausage-shaped” mass? Call 999.
Key nuance: visceral pain is *diffuse* (“somewhere down there”), while peritoneal irritation (e.g., perforation) is *sharp*, *localised*, and *worse with movement*. If yer doubling over every time ye cough? That’s not IBS. That’s “get to A&E” territory.
Inflammation Downstairs: When the Gut Throws a Proper Tantrum
“Inflammation of the lower abdomen” isn’t a diagnosis—it’s a *description*. Could be:
| Condition | Typical Location | Key Features | Linked to lower gut pain? |
|---|---|---|---|
| Diverticulitis | Left iliac fossa | Fever, leucocytosis, LLQ tenderness | Yes—classic |
| Ulcerative Colitis | Entire colon (starts rectum) | Bloody diarrhoea, urgency, tenesmus | Yes—mucosal inflammation |
| Pelvic Inflammatory Disease (PID) | Bilateral lower abdomen | Discharge, fever, cervical motion tenderness | Adjacent—can mimic |
| Appendicitis (atypical) | May present low/right | Anorexia, migration of pain, rebound | Sometimes—esp. retrocaecal |
Diagnosis? Bloods (CRP ↑), stool calprotectin (↑ in IBD), ultrasound/CT. Never assume it’s “just IBS” if it’s new, worsening, or over 50. Safety first.

Red Flags: When “Tummy Ache” Isn’t Just a Tummy Ache
Most lower gut pain is benign. But some signs? They’re your body waving a red Union Jack:
- Pain >48 hours *unrelenting*
- Fever >38°C
- Blood in stool (fresh red or black/tarry)
- Unexplained weight loss (>5% body weight in 6 months)
- Family history of bowel cancer or IBD
- Age >50 with *new-onset* symptoms
- Vomiting + absolute constipation (no wind/poo)
These aren’t “wait and see” symptoms. They’re “book a GP *today*” symptoms. Early diagnosis of IBD or cancer changes outcomes *dramatically*. Don’t Google—go see someone. Seriously.
Home Soothers: What *Actually* Helps (and What’s Just Folklore)
For *mild, recurrent* lower gut pain (think IBS or mild constipation), evidence-backed relief includes:
- Heat pad (£12.99 on Amazon): relaxes smooth muscle, eases cramping. Better than a hot water bottle (safer, consistent temp).
- Peppermint oil capsules (£8–£10 for 30): antispasmodic. Shown in trials to reduce IBS pain. *Enteric-coated only*—or it’ll burn yer oesophagus.
- Soluble fibre (psyllium husk, £4.50): bulks stool, regulates transit. *Start low*—2.5g/day—to avoid gas explosions.
- Low-FODMAP trial: 2–6 weeks cutting high-FODMAP foods (onion, garlic, beans, apples). 70% of IBS folks improve. (But *reintroduce* later—don’t stay restrictive.)
- “Where *exactly*? Point with one finger.”
- “Does it wake you at night?” (IBS usually doesn’t.)
- “Any blood? Weight loss? Family history?”
- “What makes it better/worse?” (Food? Stress? Poo?)
- https://cks.nice.org.uk/topics/abdominal-pain-lower/
- https://www.nhs.uk/conditions/stomach-ache-and-abdominal-pain/
- https://www.ncbi.nlm.nih.gov/books/NBK537098/
- https://www.gutscharity.org.uk/information/advice-fact-sheets/lower-abdominal-pain/
Skip the “flat cola and toast” myth. Sugar worsens osmotic diarrhoea. And *never* use codeine for diarrhoea-predominant pain—it can trigger toxic megacolon in IBD. Just… don’t.
When to See Someone (and What to Expect)
Book a GP if pain’s: *new*, *worsening*, *disrupting sleep*, or hitting any red flags. They’ll ask:
Exams may include PR (yes, *that*), bloods (FBC, CRP, coeliac screen), and stool tests (calprotectin, culture). If red flags? Urgent referral—2-week wait for suspected cancer, 4-week for IBD. Don’t dread it. Knowledge is power. And relief.
The Mind-Gut Axis: Why Stress Turns Your Belly into a Knot
Here’s the wild bit: yer gut’s got *more neurons than yer spinal cord*. It’s literally a “second brain”—and it chats *constantly* with the first. Stress → cortisol ↑ → gut motility ↑ → visceral sensitivity ↑ → *pain*. Ever notice symptoms flare before a big meeting or flight? That’s not coincidence. Studies show CBT and gut-directed hypnotherapy reduce lower gut pain in IBS by 50–70%. No pills. Just rewiring the chatter. Worth a look—even if it sounds a bit “woo”. Science backs it.
From Our Stables to Yours: Keep Digging, Stay Curious
Whether you’re navigating unexplained lower gut pain, decoding food reactions, or just curious how bodies *actually* work—we’re here for the long haul. Dive deeper at the Riding London homepage—your no-nonsense hub for health, science, and quietly brilliant insights. Browse our ever-growing Learn section for plain-English guides on everything from pelvic anatomy to gut microbiome myths. And if food’s your trigger, our deep-dive on gut pain after eating food intolerance clues unpacks histamine, FODMAPs, and why that avocado toast *might* be the villain. Stay curious. Stay kind to yer gut.
FAQ
What could be the cause of lower abdominal pain?
Causes of lower abdominal pain vary widely—from benign (IBS, constipation, menstrual cramps) to serious (diverticulitis, inflammatory bowel disease, ovarian torsion, bowel obstruction). In the context of lower gut pain, common GI causes include IBS (crampy, stress/food-triggered), diverticular disease (left-sided, constant), IBD (bloody diarrhoea + weight loss), and constipation (pressure, bloating). Always consider gynaecological, urinary, and musculoskeletal sources. Red flags (fever, blood, weight loss) warrant urgent evaluation.
What does pain in the colon feel like?
Colon pain is often *crampy* or *colicky* (coming in waves), localised to the lower abdomen—especially left side for sigmoid colon issues. In IBS, it eases after defecation. In diverticulitis, it’s *deep*, *constant*, tender to touch. In colitis, it’s cramping with urgency and frequent loose/bloody stools. If inflammation reaches the peritoneum (e.g., perforation), pain becomes *sharp*, *fixed*, and worsens with movement. The character of lower gut pain offers vital diagnostic clues.
What is inflammation of the lower abdomen?
“Inflammation of the lower abdomen” isn’t a diagnosis—it’s a sign. It may indicate diverticulitis (inflamed pouches in the colon), ulcerative colitis (mucosal inflammation), pelvic inflammatory disease (fallopian tubes/ovaries), or appendicitis (if atypical location). Symptoms include pain, fever, tenderness. Diagnosis requires history, exam, blood tests (CRP), and imaging (ultrasound/CT). Persistent lower gut pain with systemic signs needs medical assessment to pinpoint the source.
How do I get rid of lower abdominal pain?
For *mild, recurrent* lower gut pain (e.g., IBS), try: heat pad, enteric-coated peppermint oil (£8–£10), soluble fibre (psyllium), and a short low-FODMAP trial. Avoid codeine in diarrhoea-predominant cases. But *first* rule out red flags (blood, weight loss, fever). If present—or if pain’s new/worsening—see a GP. They may order tests (calprotectin, bloods) and refer if needed. Never self-treat serious inflammation; correct diagnosis is key to effective relief.