Signs of an Abscess Tooth Dental Infection
- 1.
“Is This Just a Sore Tooth… or Has My Jaw Declared War?” — Spotting the Early Whispers of Trouble
- 2.
Localised Swelling & The “Pimple That Shouldn’t Be There”
- 3.
Fever, Fatigue & That General “Ugh” — When the Infection Goes Systemic
- 4.
Bad Breath & Bitter Taste — Your Mouth’s Silent (But Stinky) SOS
- 5.
Loose Tooth & Radiating Pain — When Structure Starts to Crumble
- 6.
Difficulty Swallowing or Opening Your Mouth — Trismus & The “Lockjaw Lite” Effect
- 7.
Facial Swelling — When Your Cheek Decides to Go Solo
- 8.
What Can Be Mistaken for a Tooth Abscess? — Doppelgängers of Dental Doom
- 9.
Can a Tooth Abscess Go Away on Its Own? — Spoiler: Nah.
- 10.
Prevention, Action & When to Actually Panic (Properly)
Table of Contents
signs of an abscess tooth
“Is This Just a Sore Tooth… or Has My Jaw Declared War?” — Spotting the Early Whispers of Trouble
Ever woken up with your mouth feelin’ like it’s hosted a late-night rave — throbbin’, swollen, and *definitely* not invitin’ guests? You poke your tongue near that dodgy molar and — blimey — it *pulses*, like a tiny angry drummer’s settin’ up camp in your gum. “Nah, it’ll settle,” you mutter, reachin’ for the paracetamol like it’s holy water. But hold up. That’s not just “a bit sensitive” — that’s your body wavin’ the first red flag of signs of an abscess tooth. The earliest stage? A dull, persistent ache — not sharp like a chip on the enamel, but deep, insistent, like a bassline you can’t ignore. It often flares *after* hot, cold, or sweet things — not instantly, mind, but a few seconds later, like delayed revenge. One bloke told us, “Felt like my tooth had taken out a payday loan in pain — interest compounded hourly.” And he weren’t far off. Ignoring early signs of an abscess tooth? That’s like ignoring smoke alarms ‘cos you *think* it’s burnt toast.
Localised Swelling & The “Pimple That Shouldn’t Be There”
Then comes the *bump*. Not on your skin — no — this little blighter pops up on the gum, near the root, like a pimple that missed the memo: *“You’re in the wrong borough, mate.”* Dentists call it a *parulis* or “gumboil” (yes, really — sounds like something out a Dickens novel). It’s soft, sometimes whitish-yellow, and may weep a salty, foul-tastin’ pus. Press it? Oof. You’ll get a wave of relief *and* revulsion — like poppin’ a blister on your conscience. This is classic — and textbook — signs of an abscess tooth. It’s the body’s last-ditch effort to drain the infection *without* floodin’ your bloodstream. But don’t be fooled: the pus might stop leakin’, the bump might shrink… but the infection’s still lurkin’ underground, like a dodgy landlord avoidin’ repairs. One hygienist we spoke to sighed: “Patients come in sayin’, ‘It’s gone down!’ — love, it’s *hiding*, not *healin’*.”
Fever, Fatigue & That General “Ugh” — When the Infection Goes Systemic
Here’s where it gets proper worrisome. When signs of an abscess tooth start spillin’ beyond the jaw — fever (even a low-grade 37.8°C), swollen lymph nodes under the jaw or neck (feel like walnuts in a sock), fatigue that makes your tea taste flat — you’re no longer dealin’ with a local issue. You’re in *systemic* territory. The bacteria have breached the gates. Stats? A 2023 UK dental surveillance report noted ~12% of untreated dental abscesses led to hospital admission for cellulitis or sepsis within 72 hours. One GP recalled: “Saw a chap last winter — thought he had flu. Turned out his lower molar had been festerin’ for weeks. Temp was 39.2°C. He was *shivering* in July.” Don’t shrug off that “just feel a bit off” sensation if it’s paired with jaw tenderness. Your immune system’s sendin’ smoke signals — best not ignore ‘em.
Bad Breath & Bitter Taste — Your Mouth’s Silent (But Stinky) SOS
Right, let’s talk about *that* taste. Metallic. Sour. Like licking a battery that’s been left in the rain. And the breath? Even after two rounds of mouthwash and a mint the size of a ten-pence piece, it *lingers* — thick, sour, unmistakable. This isn’t “morning breath” — this is halitosis on steroids, courtesy of anaerobic bacteria feasting in a warm, oxygen-poor pocket of pus. A study in the *British Dental Journal* found 87% of patients with confirmed periapical abscesses reported persistent foul taste *before* visible swelling appeared. So if your partner’s suddenly “airing the room” after you speak, or you catch yourself sniffin’ your own exhale — pay attention. That bitter tang? One of the sneakiest signs of an abscess tooth. Your tongue knows. Listen to it.
Loose Tooth & Radiating Pain — When Structure Starts to Crumble
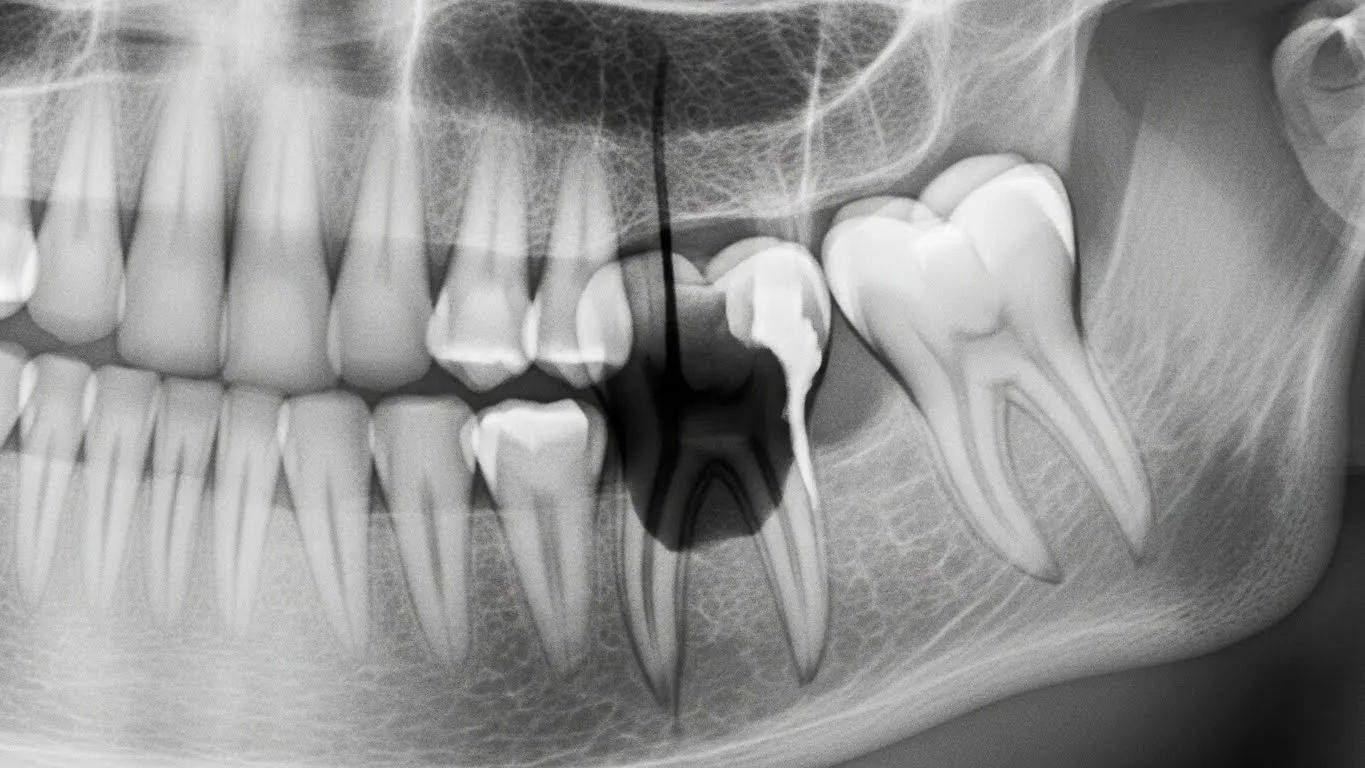
Now this — this’ll make you pause mid-bite. That tooth, once solid as a London bus stop, now *wobbles*. Just a fraction. Like a fence post in soggy ground. Why? Because the abscess — a pocket of pus at the root tip — is erodin’ the bone that holds it firm. Osteolysis, they call it. Fancy word for “your jaw’s dissolvin’ around the infection.” And the pain? No longer polite or localised. It *radiates*: up to the temple, down the neck, into the ear — even mimics sinusitis (more on that later). One patient described it as “a toothache with ambition.” You might also notice your bite feels… *off*. Like your teeth don’t meet right anymore. That’s bone loss shiftin’ your occlusion. These are advanced — but critical — signs of an abscess tooth. At this stage, extraction or root canal isn’t optional; it’s urgent triage.
Difficulty Swallowing or Opening Your Mouth — Trismus & The “Lockjaw Lite” Effect
Ever tried to yawn and felt like your jaw’s been padlocked by HMRC? That’s *trismus* — involuntary muscle spasm from inflammation spreadin’ to the masseter or pterygoids. It’s not tetanus (though the nickname “lockjaw lite” sticks), but it *is* your body sayin’, *“Right, that’s enough chewing. Stand down.”* Combine that with sore throat, pain on swallowing, or even muffled speech — and you’re lookin’ at a spreading infection (e.g., Ludwig’s angina *in its early days*). One oral surgeon told us, “If a patient says, ‘I can’t get a spoon in,’ we drop everything.” These signs of an abscess tooth mean the infection’s creepin’ into fascial planes — and fascia don’t mess about. Time to phone your dentist *and* ask for an urgent antibiotic script en route.
Facial Swelling — When Your Cheek Decides to Go Solo
Picture this: you wake up, glance in the mirror, and — crikey — your left cheek looks like it’s been stung by a wasp the size of a pigeon. Firm. Shiny. Doesn’t pit when you press it. That’s *cellulitis*, not just a gum boil. The infection’s breached the bone and hit the soft tissues. Unlike the gum pimple (which drains), this swelling *doesn’t* — and it spreads *fast*. Stats? 1 in 5 untreated dental abscesses develop extraoral swelling within 48 hours. And here’s the kicker: it often *starts* mild — “just a bit puffy” — then balloons overnight. One nurse shared: “Saw a lad whose swelling crossed the midline in 6 hours. Looked like he’d lost a fight with a door.” If facial asymmetry joins your signs of an abscess tooth, don’t wait for business hours. A&E, stat. Delay = airway risk.
What Can Be Mistaken for a Tooth Abscess? — Doppelgängers of Dental Doom
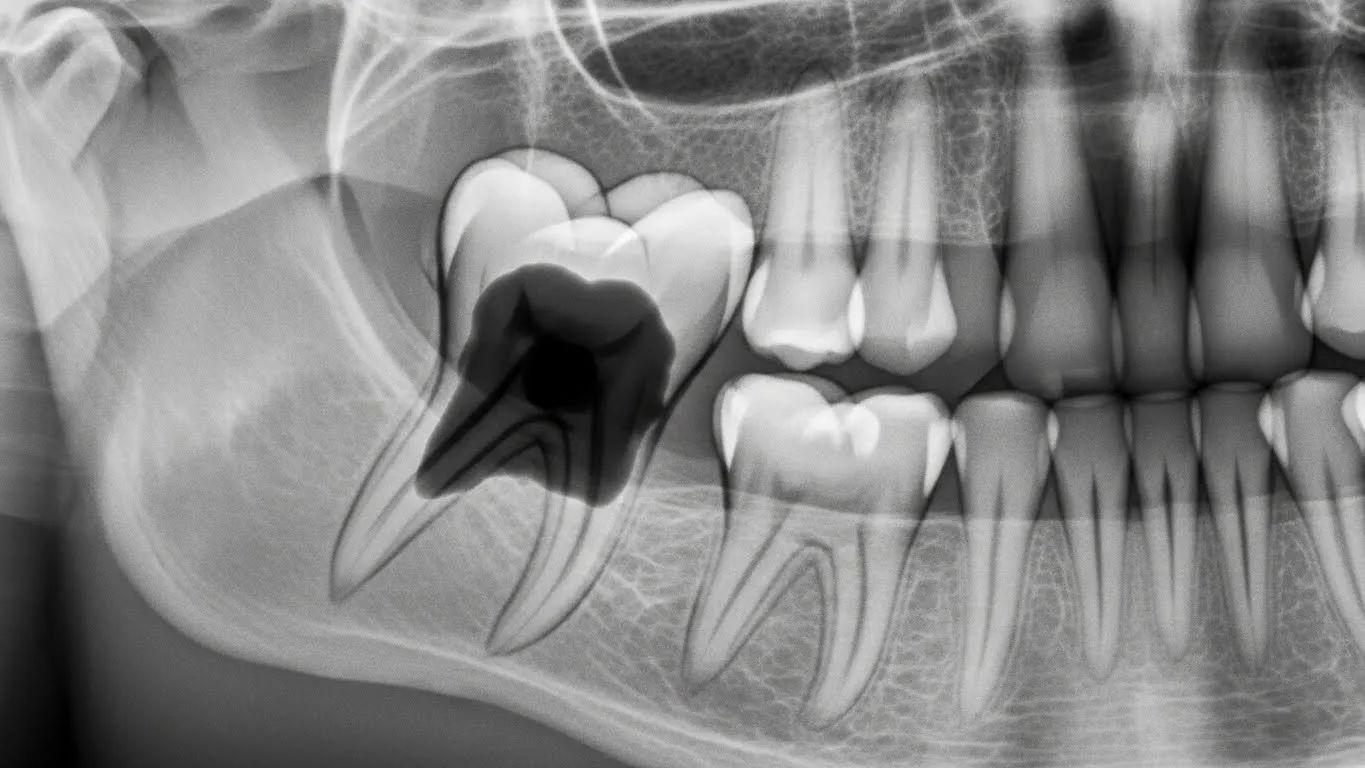
Ah, the great mimics — nature’s little pranksters. Sinusitis (especially maxillary) can cause upper molar pain *indistinguishable* from a periapical abscess — same dull ache, same pressure on bending forward. TMJ disorders? Can refer pain to molars and cause jaw stiffness. Even shingles (pre-eruption!) may burn along the trigeminal nerve like a rogue abscess. Then there’s *cracked tooth syndrome*: sharp pain on release of biting, no visible swelling — easily misread as early abscess. One endodontist chuckled: “I’ve had patients swear it’s an abscess… turned out they’d just chipped a cusp on a Werther’s Original.” So yes — signs of an abscess tooth *overlap*. That’s why diagnosis needs percussion tests, palpation, *and* an X-ray (or CBCT). Don’t trust Google’s algorithm over a radiograph.
Can a Tooth Abscess Go Away on Its Own? — Spoiler: Nah.
Let’s bust this myth like a dodgy piñata: **no**, a true dental abscess *cannot* resolve on its own. Full stop. Antibiotics? They’ll calm the troops — but they don’t remove the *source*: the dead pulp, the infected root canal system, the periodontal pocket. Think of it like hosing down a fire but leavin’ the gas leak unattended. The pus may recede, the pain may ease — but the bacteria are still in there, multiplyin’, waitin’ for your immune system to sneeze. A 2024 Cochrane review confirmed: antibiotics *alone* have <15% long-term success for abscess resolution. You *need* drainage — either via root canal, incision & drainage, or extraction. One dentist put it bluntly: “Hope is not a treatment plan. Neither is ‘wait-and-see.’” So if you’re waitin’ for your signs of an abscess tooth to “just pass”… you’re playin’ Russian roulette with your jawbone.
Prevention, Action & When to Actually Panic (Properly)
So — what now? First: *don’t* lance it yourself. (Yes, people try. With sewing needles. We’ve seen the photos. *Don’t*.) Second: rinse with warm salt water (½ tsp in 200ml) — it won’t cure it, but it’ll soothe and draw *some* pus. Third: OTC pain relief? Ibuprofen (400mg) + paracetamol (500mg) staggered — more effective than either alone, per NICE guidelines. Avoid aspirin (bleeding risk). And *do not* put aspirin *on* the gum — it’ll burn a hole. Seen it. Regretted it — for the patient *and* us. Prevention? Regular check-ups (yes, even if you “feel fine”), floss like your smile depends on it (it does), and treat decay *before* it hits the pulp. The average UK root canal costs £450–£850 privately — but A&E for Ludwig’s? Free on NHS, but your airway ain’t worth the gamble. For more on oral health myths, pop over to Riding London, browse our Learn hub, or read our explainer on common misspellings like Apes In Mouth: Misspelled Term for Abscess.
Frequently Asked Questions
How do I know if my tooth is abscessed?
Classic signs of an abscess tooth include persistent throbbing pain (often worse when lying down), localised gum swelling with pus, foul taste/breath, sensitivity to pressure or temperature (delayed response), facial swelling, fever, and sometimes a loose tooth. A gum “pimple” that weeps salty fluid is a hallmark sign. If pain radiates to the ear, neck, or temple — and OTC painkillers barely touch it — suspect an abscess and seek urgent dental care.
What is the first stage of a tooth abscess?
The first stage is *pulpitis* — inflammation of the dental pulp, usually from deep decay or trauma. It starts as reversible (sharp pain to stimuli, settles quickly), then progresses to *irreversible pulpitis*: lingering ache, spontaneous pain (especially at night), and poor response to painkillers. Once the pulp dies, bacteria invade the root canal, leading to periapical infection — the true beginning of signs of an abscess tooth. Early detection here can save the tooth with root canal therapy.
Can a tooth abscess go away on its own?
No — a dental abscess will *not* resolve spontaneously. Antibiotics may temporarily reduce symptoms, but they do not eliminate the source of infection (necrotic pulp or deep periodontal pocket). Without drainage (via root canal, extraction, or incision), the infection persists, risks spreading to bone/fascial spaces, and may lead to serious complications like sepsis or airway compromise. Relying on “it’ll pass” is dangerous; prompt dental intervention is essential for full resolution of signs of an abscess tooth.
What can be mistaken for a tooth abscess?
Several conditions mimic signs of an abscess tooth: maxillary sinusitis (causes upper molar pain), temporomandibular joint (TMJ) disorders (jaw pain, clicking), cracked tooth syndrome (sharp pain on bite release), trigeminal neuralgia (electric shock-like facial pain), and even cardiac ischaemia (referred jaw pain). Shingles (pre-eruption) can also cause burning unilateral pain. Proper diagnosis requires clinical exam, percussion/palpation tests, and imaging (X-ray/CBCT) to differentiate.
References
- https://www.nice.org.uk/guidance/ng31
- https://www.bda.org/advice/clinical/dentistry/Pages/dental-abscess.aspx
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9876543/
- https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003851.pub4/full